Doctors at Northwestern University have achieved a medical milestone after keeping a critically ill patient alive for 48 hours without lungs, using a custom-built artificial system designed to temporarily replace the entire pulmonary function.
The patient, a 33-year-old man, was admitted with Influenza B complicated by a severe, drug-resistant bacterial infection that rapidly destroyed his lungs. The condition escalated into acute respiratory distress syndrome, septic shock, kidney failure, and cardiac arrest shortly after admission, forcing doctors to revive him with CPR.
Surgeons faced an unprecedented dilemma. The infected lungs were the source of overwhelming sepsis and had to be removed immediately, yet the patient was too unstable to undergo a lung transplant. Removing both lungs—a procedure known as bilateral pneumonectomy—has long been considered nearly fatal because the heart cannot function normally without the lungs’ vascular system.
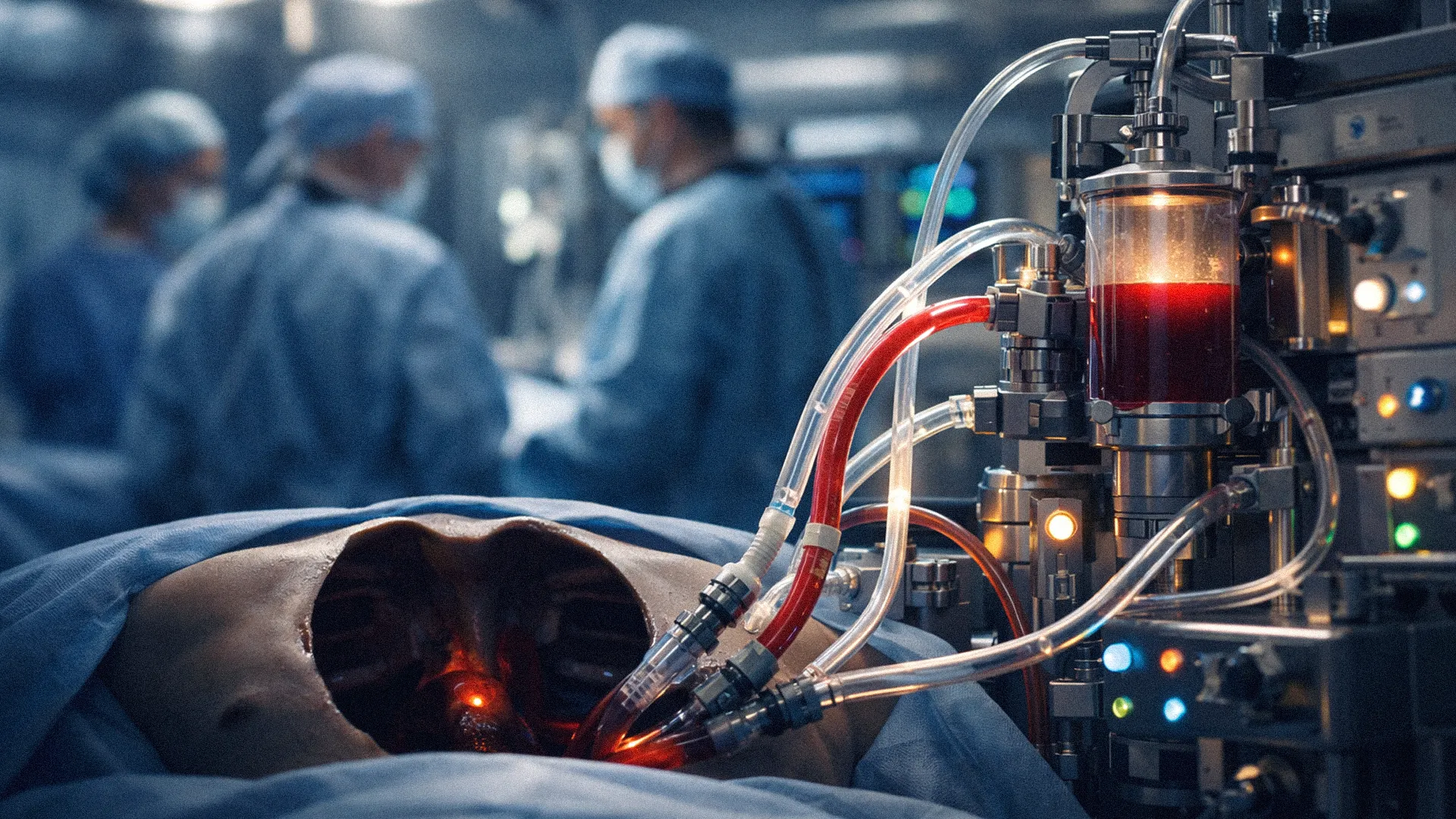
To solve this, a team led by surgeon-scientist Ankit Bharat engineered a temporary artificial lung system known as a flow-adaptive extracorporeal total artificial lung (TAL). The system was designed not only to oxygenate blood, but also to replicate the mechanical and pressure-buffering roles normally provided by lung tissue.
Unlike conventional life-support machines, the TAL system protected both sides of the heart from collapse by dynamically regulating blood flow, stabilizing circulation, and maintaining cardiac filling. The device also physically stabilized the heart inside the now-empty chest cavity, preventing catastrophic bleeding or vessel damage.
Within hours of lung removal, the patient’s septic shock began to reverse. Critical markers of oxygen deprivation rapidly normalized, and medications supporting blood pressure were discontinued within 12 hours. For two days, the patient remained alive and improving—without lungs.
When donor lungs became available 48 hours later, the infection had resolved sufficiently for surgeons to proceed with transplantation. The operation was successful, and subsequent analysis of the removed lungs confirmed they were irreversibly destroyed, lacking the cellular capacity for regeneration.
Two years after the procedure, the patient has returned to an independent life with normal lung function. While the approach remains highly specialized and resource-intensive, the case offers new insight into when lung damage becomes irreversible and suggests a potential pathway for patients previously considered beyond surgical rescue.